Introduction to Blood Flow Restriction Therapy
Blood Flow Restriction (BFR) therapy is rapidly emerging as a revolutionary approach in post-surgical rehabilitation, offering patients a way to achieve significant strength gains with notably less stress on healing tissues. This technique, which originated in Japan in the 1960s as "KAATSU training," has gained considerable scientific validation and clinical adoption over the past decade.
For patients recovering from surgery, traditional rehabilitation often presents a challenging paradox: the need to build strength while simultaneously protecting healing structures from excessive loads. BFR therapy offers a promising solution to this dilemma by allowing for significant strength and muscle mass development while using much lighter loads than conventional strength training would require.
"BFR represents a way to decrease stress placed on the joints without compromising improvements in strength, whereas for postoperative, injured, or load-compromised individuals, BFR represents a way to accelerate recovery and prevent atrophy."
As healthcare professionals increasingly seek evidence-based approaches that optimize recovery timelines and functional outcomes, BFR therapy has emerged as a valuable tool in the rehabilitation arsenal. This blog explores the growing role of blood flow restriction therapy in post-surgery rehabilitation, examining its physiological mechanisms, clinical applications, benefits, and implementation considerations.
How BFR Therapy Works: The Science Behind It
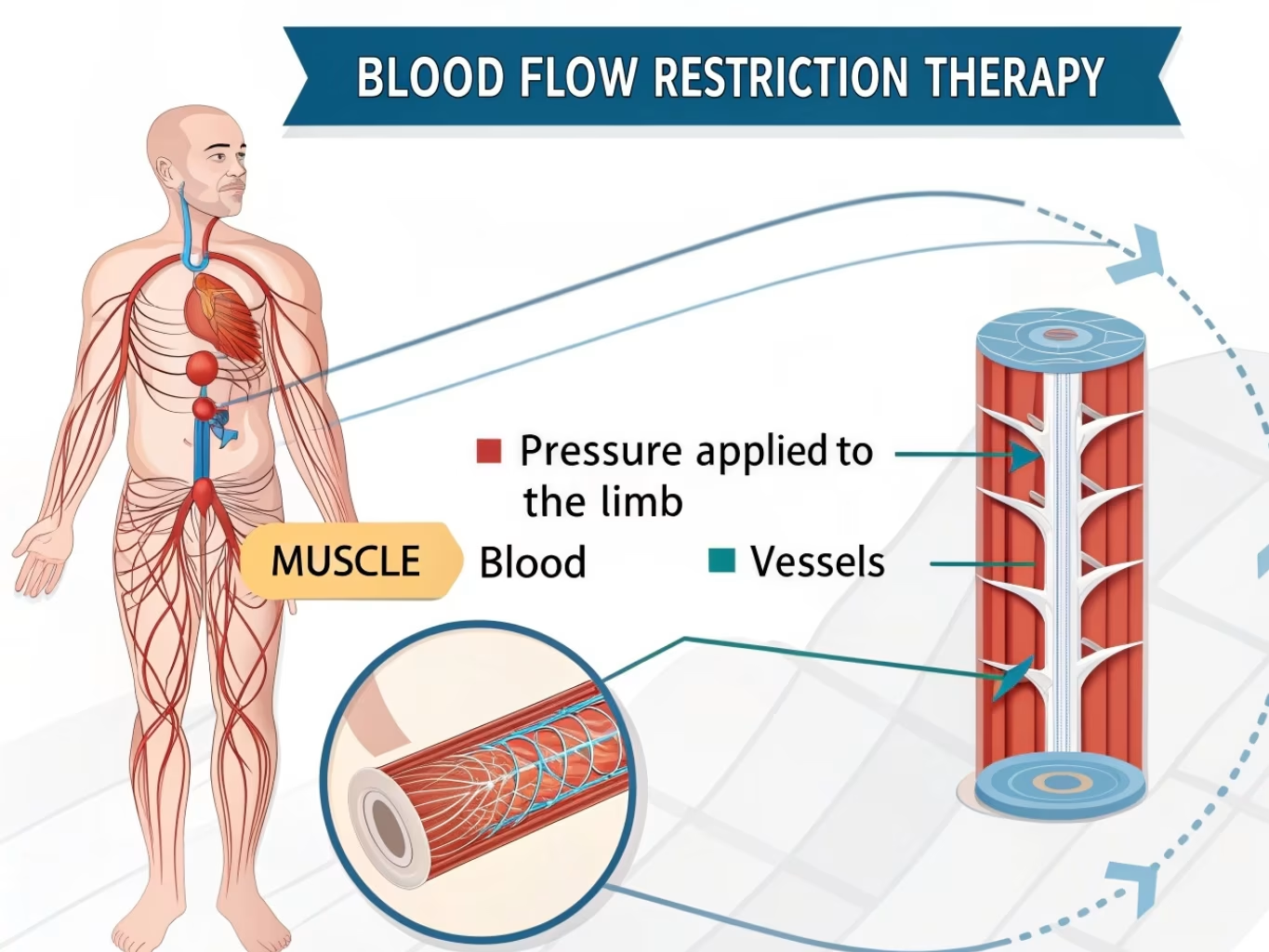
Diagram illustrating the physiological mechanism of blood flow restriction therapy
The Physiological Mechanism
Blood Flow Restriction therapy involves the application of specialized pressure cuffs or bands proximal to the muscle being trained. These cuffs are carefully adjusted to:
- Partially restrict arterial blood flow into the limb (typically allowing 25-50% of normal flow)
- Substantially restrict venous return from the limb (nearly 100%)
This controlled restriction creates a unique metabolic environment in the muscle with several key effects:
Key Cellular Responses
Metabolite Accumulation
Lactate and other metabolites build up due to restricted blood flow, creating significant metabolic stress even with light loads (20-30% of maximum).
Muscle Fiber Recruitment
Fast-twitch type II muscle fibers (typically only recruited during heavy lifting) are activated even with light loads due to the hypoxic environment.
Growth Hormone Release
Studies show that BFR triggers up to 290% increase in growth hormone levels compared to the same exercise without restriction.
Cell Swelling Response
Blood pooling in the muscle creates cellular swelling that triggers protein synthesis and inhibits protein breakdown.
The Synergistic Response
Blood flow restriction therapy stimulates muscle hypertrophy through a synergistic response to both metabolic stress and mechanical tension. This dual pathway to muscle development allows for significant strength gains without the joint stress typically associated with heavy resistance training—making it particularly valuable in post-surgical settings where protecting healing tissues is paramount.
Key Benefits of BFR in Post-Surgery Rehabilitation
Patient progress comparison showing rehabilitation outcomes with BFR therapy
Strength with Low Load
Achieve significant muscle strength gains using only 20-30% of maximum load, reducing stress on healing tissues and joints.
Accelerated Recovery
Patients can begin strengthening earlier in the rehabilitation process, potentially reducing recovery timelines.
Atrophy Prevention
Significantly reduces muscle atrophy during periods of reduced mobility or weight-bearing restrictions.
Cardiovascular Benefits
Improves vascular function and cardiac output with much less cardiovascular stress than high-intensity training.
Pain Reduction
Research indicates BFR can attenuate pain responses during rehabilitation, potentially improving exercise tolerance.
Protective of Joints
Minimizes joint stress and loading while still producing the neuromuscular adaptations needed for strength development.
Neural Adaptations
Stimulates neural adaptations that contribute to strength development even in the absence of heavy loading.
Clinical Applications of BFR Therapy

Clinical application of blood flow restriction bands during rehabilitation
Blood Flow Restriction therapy has demonstrated effectiveness across a wide range of post-surgical rehabilitation contexts. The following applications have shown particularly promising results:
| Surgical Procedure | BFR Application | Reported Benefits |
|---|---|---|
| ACL Reconstruction | Early strength training with 20-30% 1RM loads under BFR | Significantly greater quadriceps strength recovery, reduced atrophy, earlier return to function |
| Total Knee Arthroplasty | Low-load resistance training with BFR during early rehabilitation | Improved strength outcomes, increased muscle cross-sectional area, enhanced functional measures |
| Rotator Cuff Repair | BFR applied to arm exercises during protected phases | Maintained shoulder girdle strength, reduced atrophy of non-immobilized muscles |
| Meniscus Surgery | Walking and basic resistance exercises with BFR | Expedited strength recovery, reduced pain during exercise, improved functional outcomes |
| Achilles Tendon Repair | Non-weight bearing exercises with BFR during immobilization | Preservation of calf muscle mass, reduced strength deficits upon return to weight-bearing |
Beyond Orthopedic Surgery
While orthopedic applications remain the most researched, BFR therapy is also showing promise in other post-surgical contexts:
- Cardiac Rehabilitation: Low-intensity BFR training has demonstrated cardiovascular benefits with reduced cardiac stress.
- Neurological Recovery: Early research suggests BFR may enhance neural adaptations following certain neurological procedures.
- Geriatric Rehabilitation: Older adults recovering from various surgeries have shown improved strength outcomes with lower fall risk when using BFR.
Implementation Guidelines for Practitioners
Implementing BFR therapy effectively requires careful consideration of various factors to ensure safety, comfort, and optimal outcomes. Here are key guidelines for clinical implementation:
Equipment Considerations
Pneumatic Systems
Pros: Precise pressure control, automated monitoring, consistent application
Cons: Expensive, less portable, requires more setup time
Best for: Clinical settings, high-risk patients, research applications
Practical Tourniquet Cuffs
Pros: More affordable, portable, easy to apply
Cons: Less precise pressure control, potential for uneven application
Best for: Home programs, lower-risk applications, maintenance phases
Protocol Guidelines
| Parameter | Early Post-Op Phase | Mid Rehabilitation | Advanced Rehabilitation |
|---|---|---|---|
| Pressure | 40-50% LOP* for upper limb 50-60% LOP* for lower limb |
50-60% LOP* for upper limb 60-70% LOP* for lower limb |
60-70% LOP* for upper limb 70-80% LOP* for lower limb |
| Load Intensity | 20-30% 1RM | 20-40% 1RM | 30-50% 1RM |
| Sets/Reps | 3-4 sets 30/15/15/15 reps |
3-4 sets 30/15/15/15 reps |
3-4 sets 30/15/15/15 reps or 3-4 sets to fatigue |
| Rest Periods | 30-45 seconds (without releasing cuff) |
30-45 seconds (without releasing cuff) |
30-60 seconds (without releasing cuff) |
| Frequency | 2-3 times per week | 2-4 times per week | 2-4 times per week |
*LOP = Limb Occlusion Pressure (the minimum pressure needed to completely occlude blood flow)
Safety Considerations
Contraindications
- History of deep vein thrombosis or pulmonary embolism
- Active cancer or lymphedema in the affected limb
- Severe hypertension (>180/110 mmHg)
- Vascular grafts or dialysis access in the affected limb
- Severe peripheral vascular disease or varicose veins
- Sickle cell anemia
- Acute infection at cuff site
Cautions - Proceed with Modified Protocols
- Controlled hypertension
- Diabetes (with careful skin monitoring)
- History of prior venous insufficiency
- Pregnancy
- Mild peripheral vascular disease
Case Studies and Evidence-Based Outcomes
The effectiveness of blood flow restriction therapy in post-surgical rehabilitation has been documented across numerous research studies and clinical case reports. Here we highlight several key findings that demonstrate its growing impact:
Case Study 1: ACL Reconstruction
Patient Profile: 24-year-old male athlete, ACL reconstruction with hamstring autograft
Protocol: Low-load BFR training (30% 1RM) initiated 2 weeks post-surgery, 3x weekly alongside standard rehabilitation
Outcomes at 12 Weeks:
- Quadriceps strength deficit of only 15% compared to uninvolved side (vs. typical 25-30% deficit with standard rehabilitation)
- Significantly better single-leg hop performance
- Minimal graft site pain during strength training
- Cleared for return-to-sport training 4 weeks earlier than projected timeline
Greater strength recovery compared to standard protocol at 12-week assessment
Case Study 2: Total Knee Replacement
Patient Profile: 68-year-old female with total knee arthroplasty, history of osteoarthritis
Protocol: BFR walking program (20 minutes, 3x weekly) and low-load resistance training beginning 3 weeks post-surgery
Outcomes at 8 Weeks:
- 89% improvement in Timed-Up-and-Go test (vs. 62% in control group)
- Significant reduction in pain during functional activities
- Improved knee ROM and reduced swelling
- Higher patient-reported satisfaction with recovery process
Greater improvement in functional capacity compared to standard protocol
Systematic Review Evidence
A 2023 systematic review examining BFR training in post-surgical rehabilitation found that:
of studies reported superior strength outcomes with BFR vs. standard rehab
reported reduced muscle atrophy in BFR groups
reported faster functional milestone achievement
"Compared with low-load training alone, low-load BFR training is more effective, generally well-tolerated, and therefore a potential clinical rehabilitation tool for post-surgical recovery."
The Future of BFR in Rehabilitation Medicine
As research and clinical applications continue to expand, several emerging trends are shaping the future of blood flow restriction therapy in rehabilitation medicine:
Technological Advancements
- Development of wireless, portable BFR systems with pressure auto-regulation
- Integration with biofeedback and mobile applications for real-time monitoring
- Wearable BFR garments for home-based rehabilitation with remote monitoring
- Smart cuffs with embedded sensors to track physiological responses
Expanded Clinical Applications
- Integration with neuromuscular electrical stimulation for enhanced outcomes
- Application in neurological rehabilitation (stroke, TBI recovery)
- Utilization in cancer rehabilitation to combat treatment-related muscle loss
- Preoperative conditioning to improve post-surgical outcomes
Research Frontiers
Current research is exploring several exciting directions that may further expand the role of BFR therapy:
Molecular Signaling Optimization
Research into the precise molecular pathways activated by BFR to develop more targeted protocols.
Genetic Response Profiling
Investigating genetic factors that may influence individual responses to BFR training.
Tissue Healing Enhancement
Exploring how controlled ischemia and reperfusion cycles may directly enhance tissue healing beyond muscle adaptation.
Neuroplasticity Effects
Investigating how BFR might enhance neuroplasticity and motor learning during rehabilitation.
Challenges and Opportunities
Despite its promise, several challenges remain in optimizing BFR therapy for widespread clinical adoption:
- Standardization of protocols across different patient populations and conditions
- Development of clear guidelines for individualized pressure prescription
- Integration into insurance reimbursement models
- Expanded education for rehabilitation professionals
- Long-term outcome studies tracking results beyond the immediate rehabilitation phase
Addressing these challenges presents significant opportunities for improving post-surgical rehabilitation outcomes across diverse patient populations.
Conclusion
Blood Flow Restriction therapy represents a significant advancement in rehabilitation medicine, offering a scientifically validated approach to enhancing post-surgical recovery outcomes. By enabling significant strength and muscle mass development with reduced mechanical stress on healing tissues, BFR addresses one of the fundamental challenges of rehabilitation: how to build strength without compromising healing structures.
The growing body of evidence supports BFR as an effective tool for:
- Accelerating strength recovery following orthopedic surgeries
- Preventing muscle atrophy during periods of reduced mobility
- Enhancing functional outcomes with lower joint stress
- Potentially reducing overall rehabilitation timelines
- Improving patient satisfaction and exercise tolerance during recovery
As research continues to expand and technology advances, blood flow restriction therapy is likely to become an increasingly integral component of post-surgical rehabilitation protocols. Clinicians should consider incorporating this evidence-based approach into their practice while staying current with evolving best practices for implementation.
The future of BFR therapy in rehabilitation is promising, with ongoing innovations in technology, application techniques, and our understanding of its physiological effects continuously expanding its potential to improve patient outcomes.
Key Takeaways
- BFR allows significant strength gains with only 20-30% of maximum load
- The technique works through synergistic metabolic stress and mechanical tension mechanisms
- Research demonstrates superior outcomes in post-surgical rehabilitation compared to standard low-load training alone
- Proper implementation requires careful pressure and protocol customization for individual patients
- The future of BFR includes technological advances, expanded applications, and deeper understanding of its mechanisms
References
- Hughes L, Rosenblatt B, Haddad F, Gissane C. (2019). Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients. Sports Medicine, 49(11), 1787-1805.
- Hughes L, Paton B, Rosenblatt B, Gissane C. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. British Journal of Sports Medicine, 51(13), 1003-1011.
- Colapietro M, Portnoff B, Miller SJ. (2023). Effects of blood flow restriction training on clinical outcomes for patients with ACL reconstruction: a systematic review. Sports Health, 15(2), 245-253.
- Van Cant J, Dawe-Coz A, Aoun E. (2020). Quadriceps strengthening with blood flow restriction for the rehabilitation of patients with knee conditions: a systematic review with meta-analysis. Journal of Rehabilitation Medicine, 52(11), jrm00134.
- Gopinatth V, Garcia JR, Reid IK, Knapik DM. (2024). Blood Flow Restriction Enhances Recovery After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Arthroscopy: The Journal of Arthroscopic & Related Surgery, S0749-8063(24)00416-X.
- Franz A, Praetorius A, Raeder C, Hirschmüller A. (2023). Blood flow restriction training in the pre-and postoperative phases of joint surgery. Arthroskopie, 36, 162-168.



